During National Nurses Week we’d like to honor the hard work, compassion, and dedication of nursing professionals and show appreciation for their invaluable contributions to our industry. But this year, we cannot overlook the difficulties those in the industry are up against. Across the country, high burnout, low availability, and raising costs related to retention and recruiting nursing staff are making headlines. These challenges of course are related. High burnout leads to retirement, career changes, or moving to a less stressful healthcare environment.
In each of these cases, that leaves fewer nurses to fill the roles available. Nurses in a number of healthcare organizations have reached a point of frustration with staffing levels that have led to strikes in a number of states, including the largest of 2022: 15,000 nurses in Minnesota, and 7000 in NYC. “There were 385 strikes in 2022, up 42% from 270 in 2021, according to the Cornell University School of Industrial and Labor Relations. The US Labor Department, which tracks only major strikes by 1,000 or more workers, recorded 20 strikes in the first 11 months of 2022, up 33% from the same period in 2021.” Those nurses who are working have seen pay rise considerably over the past year. As of March, the average yearly base pay for hospital nurses had reached $86,674, up 9% from $79,172 in June 2021, according to Premier Inc., a healthcare consulting, contracting and data-analytics company, which analyzed salaries of about 116,000 nurses.
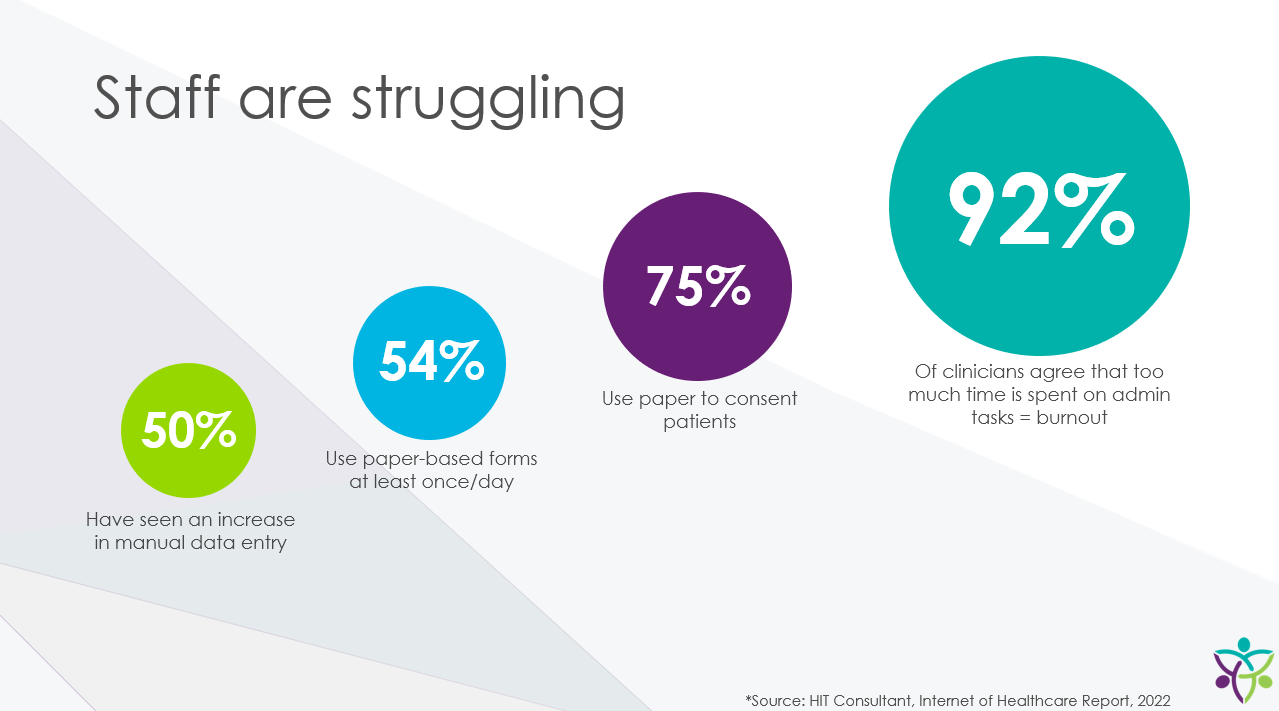
Unfortunately, the demand for nurses is increasing while the supply of nurses is decreasing – with no near-term solution in sight. In addition, with financial pressures increasing with the end of the Public Health Emergency, it’s clear health systems will need to accomplish “more with less” while avoiding pushing nursing unions to call strikes. Adding to the rising costs and a shrinking supply of nurses to staff hospitals, the amount of time being spent with patients is well below 50%. Less than one-third of registered nurses’ work time was spent with patients. They allocated the most time to the dimensions of ‘communication and care coordination’ and ‘care planning’, whereas ‘optimizing the quality and safety of care’, ‘integrating and supervising staff’, and ‘client education’ were allocated the least time.
Turning to Technology to Tackle Nursing Workloads
Although it’s a complex problem, if we can begin to address these issues now, we can guarantee a better future for nurses, patients, and providers alike. But, how can health systems accomplish this balancing act? For a number of organizations, effective deployment of technology is the best option to accomplish these goals. Below are three examples of how technology has made a positive impact on nursing staff:
1.) AI Robot Makes Strides with Nursing Staff Support
Tacoma, WA- based Multicare Health deployed Moxi – an AI enhanced Robot – earlier this year. In its first week, Moxi saved nurses and clinical staff 320,000 steps and saved 364 person-hours…all in one week! I personally have also seen Moxi in operation at Corewell Health (formerly Spectrum Health) in Grand Rapids, Michigan. It was impressive to watch several unattended deliveries take place to different patient rooms while I was visiting a relative.
Aurora, Colo.-based UCHealth launched a project to give nurses technology that provides tools to capture patient data and said it saved nurses 64,800 hours by simplifying documentation processes within its Epic EHR. The project optimized the system’s nursing documentation by reducing 18 minutes of time spent in flowsheets per nurse shift, reducing the amount of time and number of actions needed to complete documentation and cutting the required nursing documentation for the average patient by more than half.
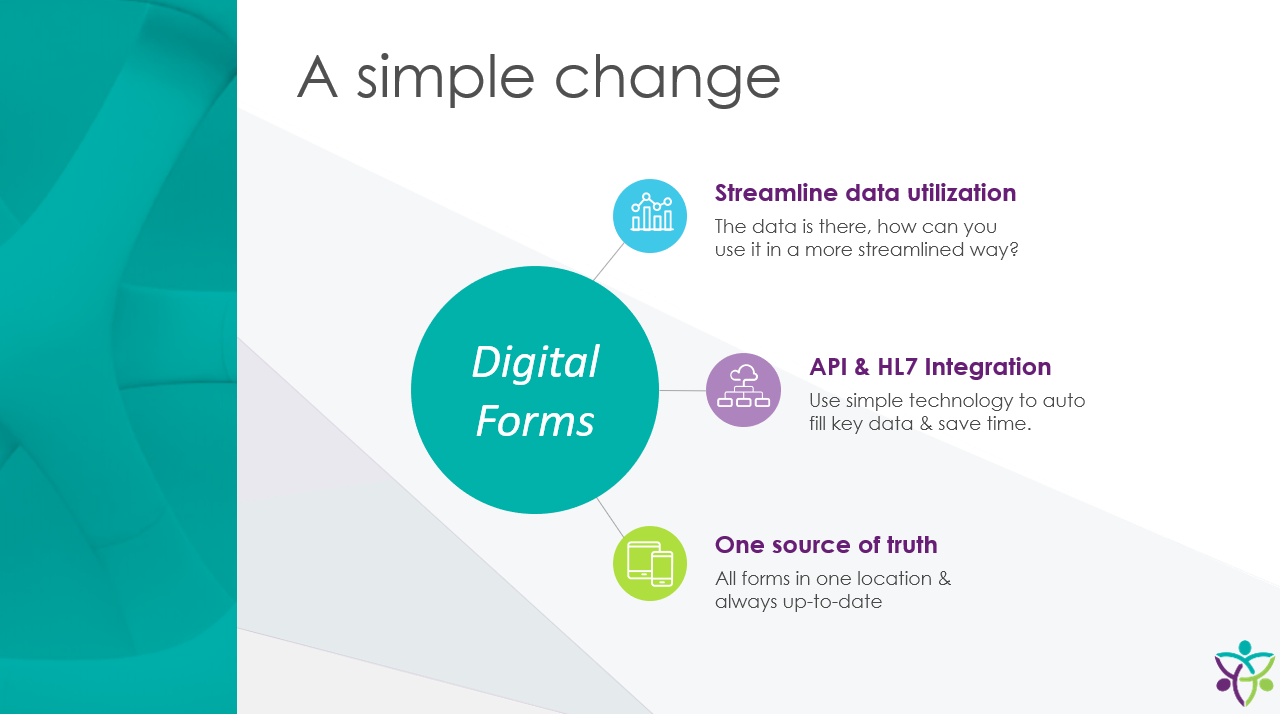
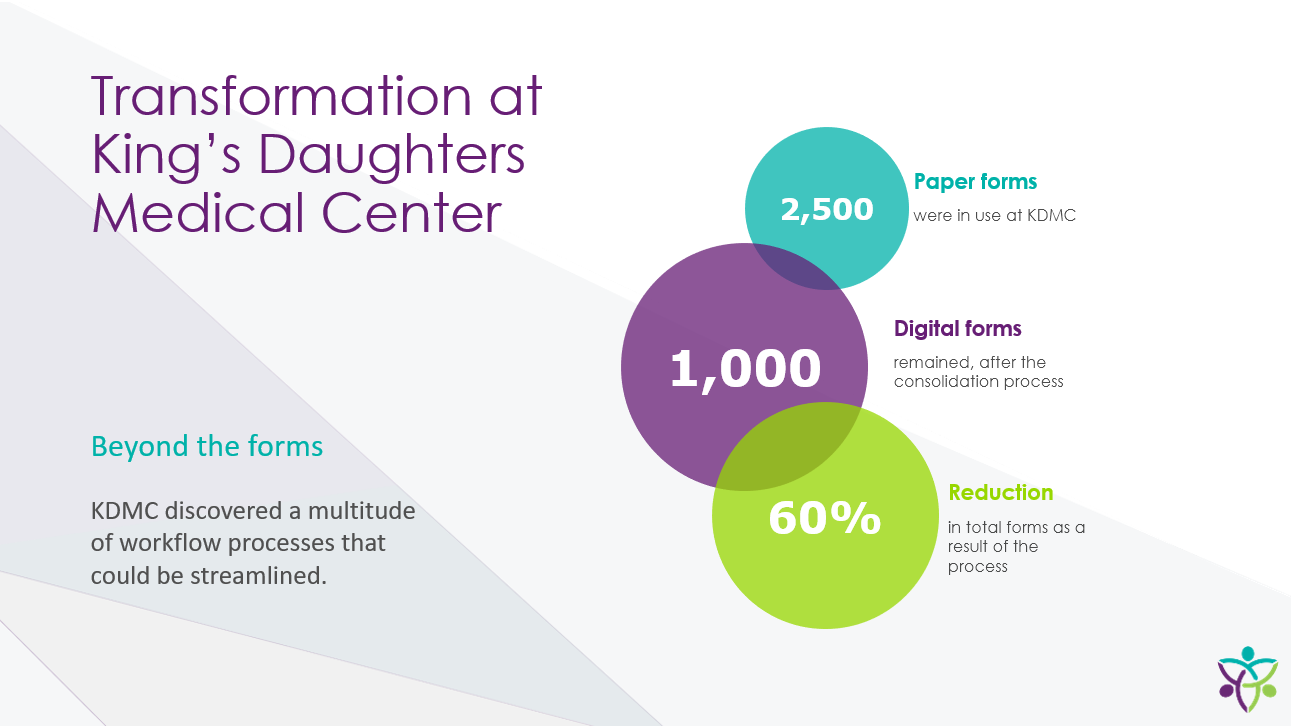
3.) Automate Informed Consent Workflow & Signature Capture
Miami, Florida-based Nicklaus Children’s Hospital replaced labor intensive paper-based consents for patients with an automated workflow provided by Interlace Health which includes EHR integration and electronic signature capabilities. Leveraging iPad tablets and Interlace Health software, Nicklaus estimated they saved 4914 hours of nursing time. How are these hours saved at this regional pediatric hospital? The surgery department is the primary option for patients in the region, so they have a high volume of surgeries. They are required to collect informed consent the day of the surgery or procedure and so the nurses are responsible for printing the necessary forms and putting them into the chart. They are later scanned, filed, and shredded. This amounts to thousands of pieces of paper and over four-thousand hours of nurse time.
With the implementation of eSignature for Informed Consents the entire process is condensed. During pre-op, the nurse launches the consent forms on either a computer or tablet, and all the patient and provider information related to the procedure is automatically populated. The physician comes in and reviews the consent with the patient guardian and both sign right then using the touch screen. The time and date are applied electronically, and the form is locked from any future edits and instantly archived to the EHR. Copies can later be emailed to the patient. During timeout, the physician confirms consent was collected and they begin the procedure.
There is no paper trail related to the consenting of these patients. Those nearly 5000 hours of nurse time are repurposed for patient care. All three of these examples, highlight how technology reduces the amount of time nurses spend on tasks not consistent with operating at top of licensure. Thousands of hours in each of these systems, have been redirected towards patient engagement and care. Additionally, with nursing costs ranging from $29.11 in South Dakota to $59.62 in California, the financial return on investment of these technologies can be quite high.
What do these three projects have in common? Close collaboration among Nursing Leadership such as CNOs and CNIOs, the CIO’s office and vendor partners were critical to their success. Tackling time-intensive administrative tasks is not an option or nice to have, these solutions are “must haves”. While hours costs may be flattening, the overall labor supply for nursing is only getting worse.
The Time for Change is Now
A recent report from McKinsey predicts potentially dire nurse staffing issues in the next few years, as the nationwide nursing shortage could reach 450,000, or 20 percent, by as early as 2025. This same report noted that 90% of hospitals are unable to increase surgery volumes due to limited nursing staff, impacting the ability to grow revenues and offset cost pressures.
Last year, for the first time in 20 years, nursing school enrollment decreased, right at the time when it needs to be increasing by double digits. The current staffing challenge will only get worse without increasing productivity. Technology can be the key to help harmonize workflows, automate documentation processes, and simplify communication to create optimal work environments for nurses.
Interlace Health is dedicated to providing solutions that put people over paperwork (now and in the future) – with critical nurses and clinicians at the top of our list of staff whose workflows we aim to improve through automation.
About the Author:

Art Nicholas, Chief Commercial Officer at Interlace Health, has over 20 years of experience in launching and expanding technologies in the healthcare field. He was a pioneer in getting speech recognition used by both doctors and nurses in inpatient and outpatient settings. In every role, his teams have successfully implemented automated workflows which benefit patients, providers and the healthcare ecosystem. A strong believer in the healthcare IT community, he has been an active member of CHIME, HIMSS, and MUSE, sitting on a number of their committees. He is committed to improving the quality of patient care and lowering the cost of care delivery through well-designed and well-supported technology workflow solutions.
Learn how Nicklaus Children’s redeployed 4,914 hours of nurse time!











 Over the past five years,
Over the past five years,